
Cofounder, advocate and patient representative with ME Advocates Ireland's Joan Byrne focuses on ME in paediatrics in her written piece for the
Awareness and Educational event at Leinster House, Dublin
on the 24th January 2018.
Joan was too unwell to attend on the day, in her place MEAI's Camilla Cruise kindly read out her presentation, listen to Joan's presentation read by Camilla, go to 35 minutes into the video recording (5 minutes).
Here is the written piece by Joan here:


What
is Myalgic Encephalomyelitis?
M.E. is an acquired complex
neurological disorder affecting multiple systems of the body.
Many cases are preceded by a viral
infection with onset being usually rapid (acute).
Affected individuals do not recover
from the infection and instead experience a wide variety of symptoms including
the body’s inability to produce energy.
Energy is needed to fuel the body’s
internal functions. Cells cannot survive without energy production.
Cells need energy to perform
functions such as growth, repair, reproduction, movement, cognitive function
and defence.
All body organs work through
receiving an energy supply. If the supply is impaired in any way the body’s
organs deteriorate.
When the body receives energy it is
converted into Adenosine triphosphate (ATP) which is the energy currency of
life. It is the high-energy molecule that stores the energy we need to do just
about everything we do.
Similar to Multiple Sclerosis,
patients with Myalgic Encephalomyelitis share many similar pathologies
including impaired ATP.
Is
M.E. the same as Chronic Fatigue Syndrome?
M.E. is an acquired complex
neurological disorder affecting multiple systems of the body and appears in
medical literature from the 1950’s.
It was classified by the WHO in 1969
under Neurology G.93.3
People with M.E. have acute onset,
post infection, brain inflammation and marked debilitating Post Exertional
Malaise (PEM) after any physical or cognitive activity requiring energy
M.E. is a spectrum disease with
sufferers ranging from a mild/moderate form to profoundly severe
M.E. presents with multi systemic
symptoms similar to autoimmune illnesses
CFS is a new term made up by the CDC
in America to describe an outbreak of an M.E. type illness in Lake Tahoe in the
80’s.
Different criteria from the M.E.
criteria were used to assess patients and ‘diagnose’ them
Ignored the encephalitic
(inflammation of the brain) features of the disease and focused only on fatigue
Over time more and more people with
fatigue as their main symptom got a diagnosis of CFS
The CDC coined the hybrid term
ME/CFS which has no official coding under the WHO
Who
gets ME?
There are an estimated 12,000 to
14,000 people living with ME in Ireland. These figures are extrapolations based
on data in other countries as there is no official collation of data on
prevalence here in Ireland
Anyone can get ME at any time. From
children to adults, across all classes, creeds and colours. My own son
contracted it when he was 12 years old
ME often follows an acute viral
infection or other pathogen which then triggers the condition in some people.
They simply never recover and go on to develop many complications
75% of those with ME have a mild to
moderate degree of the condition usually meaning they are unable to lead a
normal life, gain useful ongoing employment, etc
25% of those with ME have a severe
form of the disease with many being bedbound, tube fed, unable to speak, in
intolerable pain and with serious consequences from the slightest exertion,
light or noise
Diagnosis
– the start of the problem
Diagnosing those with M.E. is not
difficult but it does take expert clinical knowledge and the right testing to
ensure accuracy. There are correct, contemporary frameworks for this (ICC-2011)
The HSE currently conflate the two
terms M.E. and C.F.S. and as a result
there are undoubtedly many patients with ME, misdiagnosed with CFS, in
the system
HSE normally blindly follow the NICE
guidelines in the UK for treatment and in the case of ME these have proved to
be profoundly incorrect and harmful to patients.
NICE are currently undertaking a
review of their guidelines for this illness, which is to be welcomed. However
it wont be finalised until 2020.
We shouldn’t have to wait til the
conclusion of that review. We can conduct our own review involving patients, patient
organisations and relevant clinicians. The expertise is amongst patients and
patient organisations.
Many
clinicians still hold the belief that M.E. is a psychological condition
(despite there being absolutely NO evidence to support that hypothesis)
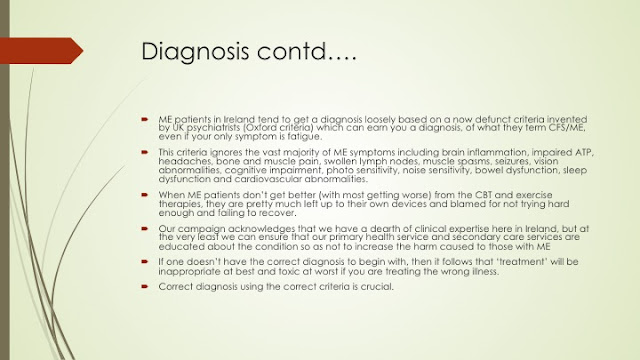
ME patients in Ireland tend to get a
diagnosis loosely based on a now defunct criteria invented by UK psychiatrists
(Oxford criteria) which can earn you a diagnosis, of what they term CFS/ME,
even if your only symptom is fatigue.
This criteria ignores the vast
majority of ME symptoms including brain inflammation, impaired ATP, headaches,
bone and muscle pain, swollen lymph nodes, muscle spasms, seizures, vision
abnormalities, cognitive impairment, photo sensitivity, noise sensitivity,
bowel dysfunction, sleep dysfunction and cardiovascular abnormalities.
When ME patients don’t get better
(with most getting worse) from the CBT and exercise therapies, they are pretty
much left up to their own devices and blamed for not trying hard enough and
failing to recover.
Our campaign acknowledges that we
have a dearth of clinical expertise here in Ireland, but at the very least we
can ensure that our primary health service and secondary care services are
educated about the condition so as not to increase the harm caused to those
with ME
If one doesn’t have the correct
diagnosis to begin with, then it follows that ‘treatment’ will be inappropriate
at best and toxic at worst if you are treating the wrong illness.
Correct diagnosis using the correct
criteria is crucial.
Current
‘treatment’ pathways for ME
Referrals of M.E. patients are
invariably made to Psychiatry and Physiotherapy with the aim of providing a
programme of Cognitive Behaviour Therapy (CBT) and Graded Exercise Therapy
(GET)
There is no evidence of these treatments
working for people with M.E. and there is much evidence that they actually harm
people with M.E. often tipping patients into a severe form of the disease
Inappropriate referrals inevitably
set up inappropriate care pathways and can end up blocking appropriate medical
investigations & multi symptom management as well as other treatment
options for those with ME
GET has been proven to seriously
harm those with ME who have extreme ATP impairment and whose bodies fail to
reproduce cellular energy used during exertions (see Journal of Health
Psychology Special edition August 2017)
GET has been removed by the CDC as a
recommended treatment but it still remains here despite the welcome move by the
HSE to remove their website information on it. This needs to be followed up
with clear up to date information to GPs and other specialities
Special
needs of Children with ME
Children as young as 4 years of age
have developed ME but the most common period of onset in young people is from
about the age of 12 to 17 yrs
Many children who are simply too
unwell to attend school have been incorrectly labelled as having ‘school
phobia’ or school avoidance issues. This label conveniently fails to explain
the fact that these children cannot take part in anything else unrelated to
school - like weekend activities,
sports, play etc.
Labelling a sick child with school
phobia can have a very damaging effect on their well being and is extremely
stressful on families and carers
Young people tend to have a better
prognosis for recovery than adults but if recovery doesn’t happen within the
first three to four years, then it is unlikely that full health will ever be
regained
Children with ME will always
seriously fall behind in school attendance.
What
do we need?
Your support to help pressurise the
HSE and relevant agencies to establish a working group on MyalgicEncephalomyelitis, with patient and patient organisation involvement
This working group’s terms of
reference should include, but not be limited to
Adopting the
internationally accepted set of diagnostic criteria (ICC-ME) which is
sufficiently rigorous to ensure correct diagnosis
Review and adopt
an internationally accepted clinical primer for adults and children with ME
Establish a
mechanism for gathering true data on the numbers of those with ME in Ireland
Developing
protocols for people with ME within hospital settings, home care settings,
community care and primary care settings, social work and educational settings
etc.
The feasibility
of appointing a Consultant with extensive experience of M.E. who will guide and
inform the development of HSE practice in line with the ICC-ME
Establishing a
process where clinicians and relevant personnel will be kept up to date with
latest research on ME emerging from international settings
Take
a moment…..
We have lost far too many people to
this disease
Deaths from cancer, heart problems
and suicide are among the top three causes of death of people with M.E.
Patients choosing to end their lives
do not want to die, but they cannot live with the unrelenting symptoms coupled
with the fact that there is no significant change on the horizon. Combine this
with neglect and abuse they often receive by those who disbelieve their
illness, think its all in their head and that they are either shirkers or have
a psychiatric problem that needs to be dealt with.
These ‘beliefs’ can have a profound
impact when trying to access financial and other disability supports for people
with M.E.
I will leave you with the words of
one ME advocate from Sweden, Anne Ortegren, who chose assisted dying in
Switzerland two weeks ago because she could simply not bear her suffering any
more but, more to the point, could not bear to think what was ahead of her.
Anne is one of too many that we have
lost to this illness. We need your help
Excerpt
from Anne Ortegren’s letter to the ME community
Nobody can say that I didn’t put up
enough of a fight.
For 16 years I have battled
increasingly severe ME/CFS. My condition has steadily deteriorated and new additional
medical problems have regularly appeared, making it ever more difficult to
endure and make it through the day (and night).
Throughout this time, I have
invested almost every bit of my tiny energy in the fight for treatment for us
ME/CFS patients. Severely ill, I have advocated from my bedroom for research
and establishment of biomedical ME/CFS clinics to get us proper health care.
All the while, I have worked hard to find something which would improve my own
health.
We still don’t have in-patient
hospital units adapted to the needs of the severely ill ME/CFS patients.
Funding levels for biomedical ME/CFS research remain ridiculously low in all
countries and the erroneous psychosocial model which has caused me and others
so much harm is still making headway.
Anne’s words contd…
And sadly, for me personally things
have gone from bad to worse to unbearable. I am now mostly bedbound and
constantly tortured by ME/CFS symptoms.
This means I no longer see a way out
from this solitary ME/CFS prison and its constant torture. I can no longer even
do damage control, and my body is at the end of its rope.
Therefore, I have gone through a
long and thorough process involving several medical assessments to be able to
choose a peaceful way out: I have received a preliminary green light for
accompanied suicide through a clinic in Switzerland.
Anne’s words contd…
When you read this I am at rest, free from suffering at last. I have written this post to explain why I had to take this drastic step. Many ME/CFS patients have found it necessary to make the same decision, and I want to speak up for us, as I think my reasons may be similar to those of many others with the same sad destiny.
These reasons can be summed up in three headers: unbearable suffering; no realistic way out of the suffering; and the lack of a safety net, meaning potential colossal increase in suffering when the next setback or medical incident occurs.
As for most other ME/CFS patients who have chosen suicide, depression is not the cause of my choice. I am not depressed. I still have all my will and my motivation. I still laugh and see the funny side of things, I still enjoy doing whatever small activities I can manage.
During these 16 years, I have never felt any lack of motivation. On the contrary, I have consistently fought for solutions with the goal to get myself better and help all ME/CFS patients get better. There are so many things I want to do, I have a lot to live for. If I could only regain some functioning, quieten down the torture a bit and be able to tolerate clothes and a normal environment,
Unbearable
Suffering – Reason 1
Many of us severely ill ME/CFS
patients are hovering at the border of unbearable suffering. We are constantly
plagued by intense symptoms, we endure high-impact every-minute physical
suffering 24 hours a day, year after year.
I see it as a prison sentence with
torture. I am homebound and mostly bedbound – there is the prison. I constantly
suffer from excruciating symptoms: The worst flu you ever had. Sore throat,
bronchi hurting with every breath. Complete exhaustion, almost zero energy, a
body that weighs a tonne and sometimes won’t even move. Muscle weakness,
dizziness, great difficulties standing up. Sensory overload causing severe
suffering from the brain and nervous system. Massive pain in muscles, painful
inflammations in muscle attachments. Intensely burning skin. A feeling of
having been run over by a bus, twice, with every cell screaming. This has got
to be called torture.
It would be easier to handle if
there were breaks, breathing spaces. But with severe ME/CFS there is no minute
during the day when one is comfortable. My body is a war zone with constant
firing attacks. There is no rest, no respite. Every move of every day is a
mountain-climb. Every night is a challenge, since there is no easy sleep to
rescue me from the torture. I always just have to try to get through the night.
And then get through the next day.
No
realistic way out of the suffering – Reason 2
A very important factor is the lack
of realistic hope for relief in the future. It is possible for a person to bear
a lot of suffering, as long as it is time-limited. But the combination of
massive suffering and a lack of rational hope for remission or recovery is
devastating.
One vital aspect here is of course
that patients need to feel that the ME/CFS field is being taken forward.
The
lack of a safety net when a setback or a new medical incident occurs – Reason 3
The third factor is the insight that
the risk for further deterioration and increased suffering is high.
For all ME/CFS patients, the
characteristic symptom of Post-Exertional Malaise (PEM) with flare-ups of our
disease when we attempt even small activities, is hugely problematic. Whenever
we try to ignore the PEM issue and push through, we immediately crash and become
much sicker. We might go from being able to at least get up and eat, to being
completely bedbound, until the PEM has subsided. Sometimes, it doesn’t subside,
and we find ourselves irreversibly deteriorated, at a new, even lower baseline
level, with no way of improving. PEM is not something that you can work around.
For me, new medical complications
also continue to arise, and I have no way of amending them. I already need
surgery for one existing problem, and it is likely that it will be needed for other
issues in the future, but surgery or hospital care is not feasible for several
reasons.
Just imagine the effects of a
hospital stay for me: It would trigger my already severe ME/CFS into new depths
– likely I would become completely bedbound and unable to tolerate any light or
noise
Anne’s plea to decision makers – Give ME patients a future!
If you are a decision maker, here is what you urgently need to do: You need to bring funding for biomedical ME research up so it’s on par with comparable diseases
You need to make sure there are dedicated hospital care units for ME inpatients in every city around the world.
You need to establish specialist biomedical care available to all ME patients; it should be as natural as RA patients having access to a rheumatologist or cancer patients to an oncologist. You need to give ME patients a future.
~ Joan Byrne














No comments:
Post a Comment