"Clinical descriptions of diseases have a way of protecting those of us who are doctors from the intensity of suffering our patients actually experience. I have always wished that doctors could learn about disease directly from patients...."
.jpg) |
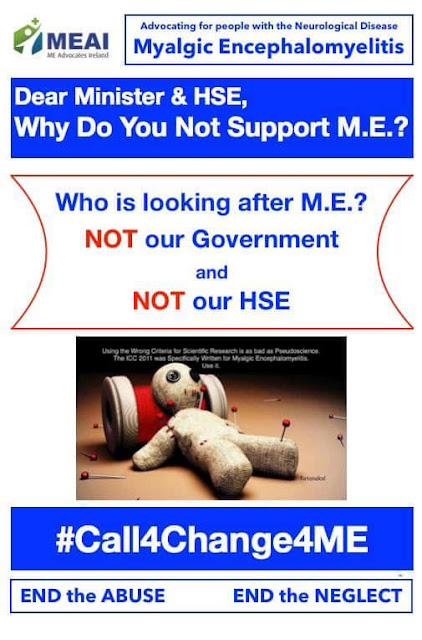
| Image by MEAI |
- THERE IS NO KNOWLEDGE AMONGST GPs
· It is potluck as to the GP’s ‘belief’ of what ME is, is it organic, does it have a specific pathophysiology, is it psychological or is ‘the patient’ not-coping with life?
· Many medics do not regard ME as an organic presentation.
· Most have no knowledge of the pathophysiology of ME, their reference is ’fatigue’.
· Attitudes to Service Users range from supportive on a person-centred level to dismissive and blaming for not ‘making an effort as there’s nothing wrong with you’.
· Standard bloods come back within lab range. No knowledge of issues with low in range results or too high in range.
· ME appropriate tests are not done, e.g., NASA lean test and others mentioned in the ICP.
· GPs have no idea of a referral pathway to an ME knowledgeable Consultant; some ask their patients if they know who to refer them to.
· Treatment/management of ‘obvious symptoms’ is not based on an understanding of the pathophysiology of ME.
· No knowledge of the concept of post exertional neuroimmune exhaustion (PENE) whereby as energy supply decreases the body’s functions shut down to enable the essential organs of survival to function.
· GPs seem unaware of the severity of ME as patients attending a GP are mild or moderate or are those within the more severe categories who use their ‘one off mind over matter’ energy to get to and from the surgery, but then experience the exacerbation of symptoms which PENE triggers for a period of time making the basics of daily life such as food, fluids and heat pushing the person further into PENE.
· Those at the most severe end of the ME spectrum, the severely and profoundly ill ‘do not exist’ as they cannot attend a surgery. House visits are ‘unusual’, and many GPs have no understanding of the needs of a person with severe/very severe/profound ME, certainly ME is not seen as a reasonable reason for a house call.
Those at the lowest end of the ME spectrum are invisible to the health services.
· GPs seem unaware that the quality of life of people with ME is the lowest of ANY chronic illness.
· Many GPs believe children ‘can’t get ME’.
· Parents with children with moderate ME are encouraged to push their child into ‘normal’ activities, which, given the pathophysiology of ME creates a high probability of deterioration.
· GPs refer children to Paediatricians in local hospital groups, where the same lack of knowledge and attitudes referred to with reference to GPs are found.
· Referrals to the Children’s Hospital Group raise further issues as the group continues to advocate CBT & GET, both designed to dismiss and deny the child’s experiences of their body by requiring them to ‘push through the warning signs as they are unhelpful illness beliefs’’ which has the potential to cause psychological harm to a child who is ill.
· A further issue arises when school attendance falls below accepted levels, as neither EWO’s, Social Services or Tusla understand ME or the potential for causing harm by forcing a child to attend school when they are struggling to manage the basics of daily life.
· The lack of GP knowledge means that the ‘early’ support system which contextualises the clinical presentation and defines, through discussion with the child and the family, what is and is not possible in terms of activity, is absent. This lack of clinical support and guidance to those in community services leaves a family and the child without the supports they needs and in fear of the uninformed judgements being made about them, therefore their problem is increased by both health and social services rather than them being supported.
· This absence of clinical context provided by the GP increases the risk of harm, to the child, possibly causing permanent harm, and lowers the opportunity for remission/recovery which a child, effectively managed, has a greater chance of achieving than an adult.
· Once a child is of an age to leave Children’s services, there is no ‘joined up’ service provision or referral route. Many Paediatricians retain their patients beyond the age ‘cut off point’ as there is nowhere to send them.
· For those who are referred to adult services there is no transfer of files from Paediatric to Adult services. Files are simply closed and stored away so for those with ME it is like starting the journey, into the unknown, all over again.
· The risk of poor experiences in Paediatric services due to having ME can result in caution/fear when entering Adult services given the lack of knowledge or consistency in acknowledgment that ME is a WHO Classified neurological disorder.
- THERE IS NO KNOWLEDGE AMONG CONSULTANTS/ SPECIALISTS
· If a person is referred to a Consultant, the common experiences are as with a GP.
· Neurologists, Cardiologists and Rheumatologists etc. largely dismiss the aspects of ME which sit within their specialities as they do not meet the threshold for intervention according to their clinical guidance.
· Without the involvement of a clinician who understands the complexity of ME as it affects all systems and organs, the attempts of one speciality or another to address one aspect of a presentation or ‘a symptom’ can lead to further imbalance or a further experience of ‘nothing to see here’ and dismissal.
The HSE’s often stated response that people with ME are given ‘symptom management’ can reasonably be stated to be an act of neglect. The ME Community is an unusual one as they have no HSE ‘Champion’ or even anyone with an interest in ME that the HSE can identify.
· Many people have been forced to see a psychiatrist or to follow a mental health route. Not because they are having mental health issues beyond the norm of those living with a misunderstood severe chronic illness, but because the power of the clinical establishment is such that that is the ‘easy way’ to ‘do something’.
· Many parts of life require a supporting letter from a Consultant, for insurance, disability, retirement on ill health, access to disability services, blue badge.
· It is hard enough for those assigned to a disease specific Consultant or one knowledgeable about their illness to overcome the barriers living with disability provides. Having ME adds a further barrier and inequality, as many have no access to a Consultant, and for those that do, there is no knowledge of the underlying pathophysiology which can be emphasised to support an application as listed above.
· Access to support in the home, care, adaptation grants etc all benefit hugely from the support of a Consultant, but for most with ME, this support is unavailable.
· Consultant support for those who cannot leave their homes is absent.
· Collectively, we have met only two Consultants who ‘speak the language’ of ME and have some grasp of the complexity of the disorder and the dreadful toll it takes on the life of the individual sufferer and their families. But they are not ME consultants and have other roles which takes from there potentially being a knowledgeable ME Consultant available fulltime. With the numbers with ME it is not practical that we continue to do without ME champions in each CHO.
· How many people with ME avoid hospitals and acute services as they do not believe the investment of their energy to attend or be admitted will pay any dividends?
· How many people with ME have experienced harm and have deteriorated due to an admission?
· ED too often evidences a dismissive response from staff, a denial of the illness or even any awareness that it exists and denigration of the person with ME is all too often a reported outcome.
- THERE IS NO NATIONAL POLICY ON ME
In the absence of clinical guidance on ME, acute and community staff have no lead, nowhere to turn. It is recommended that a national guidance document for ME should be developed by the HSE to provide information and guidance regarding the condition with information in relation to the care and support available through the HSE to sufferers.
- THERE IS NO RECOGNIZED SET OF CRITERIA USED BY THE HSE
In the absence of clinical criteria on ME, acute and community staff have no lead, nowhere to turn.
It is recommended that the HSE adopt robust criteria such as the International Consensus Criteria, 2011.
- THERE IS NO TRAINING IN MED SCHOOLS
- THERE IS NO EDUCATION AMONG MEDICAL PROFESSIONALS
When will the HSE & Government become sufficiently aware of the harm being done to adults, and to children and families across the country who are suffering due to the lack of knowledge of ME?
Until there is an objective framework of standards, based on a sound and quality evidence base, there can be no accountability.
How can the HSE hope to address a situation if it does not know what the territory is?
Qualitative and quantitative data are required for the HSE to understand the complexity of the current situation re ME.
Government health departments “worldwide” need to take responsibility for this massive injustice that has left ME patients without appropriate healthcare, thus afflicting them with the poorest quality of life than most major diseases (some of which aren’t nearly as common).
There are millions of people with ME suffering year after year, decade after decade with no end in sight.
ME-supportive Specialists in Ireland
There are two supportive specialists with an interest in ME, a consultant in Dublin and another in Tullamore who care for and support many from the ME patient community. There has been positive feedback about both medics from the ME Community.
Please get in touch by emailing info@meadvocatesireland.com if you require further information and contact details for the above-mentioned medics.
ME – Supportive Specialists in the UK who visit Ireland &
see patients here
Dr Nigel Speight - is a semi-retired doctor based in England
who specialises in Paediatric ME. Dr Speight is the paediatric medical advisor
to the northern Irish ME charity Hope 4 ME & Fibromyalgia and makes regular
visits to provide consultations for children or young people. He can help with
diagnosis. He is co- author of the International Consensus Criteria, co-author
of Paediatric Primer in Frontiers in Paediatrics, and also advisor to the 25%
ME Group. He has been outspoken about the risks to children with ME being
misdiagnosed as having a psychiatric condition
Dr William Weir - is an Infectious Disease Physician,
medical advisor and a retired NHS physician who has treated ME patients for
many years and who still sees them privately. He operates a clinic in Belfast,
Northern Ireland from time to time.
Dr Speight and Dr Weir have highlighted the damage caused to
ME patients by treatments based on the view that ME results from abnormal
illness beliefs and exercise phobia and give hope that this view will soon be
replaced with scientific evidence-based medicine.
Images by ME Advocates Ireland (MEAI)

.jpg)

No comments:
Post a Comment