.jpg) |
1.17.11Monitor people with severe or very severe ME/CFS who are at risk of malnutrition or unintentional weight loss because of:
restrictive diets
poor appetite, for example linked with altered taste, smell and texture
food intolerances
nausea
difficulty swallowing and chewing.
Follow the recommendations on screening for malnutrition and indications for nutrition support, in the NICE guideline on nutrition support for adults.
1.17.12Give advice to support people with severe or very severe ME/CFS, which could include:
eating little and often
having nourishing drinks and snacks, including food fortification
finding easier ways of eating to conserve energy, such as food with softer textures
using modified eating aids, particularly if someone has difficulty chewing or swallowing
Why: The reasons can be an inability to swallow, severe gastrointestinal problems tolerating food or the patient being too debilitated to eat and drink.
How to Support: Some patients with very severe ME will require tube feeding, either enterally or parenterally.
Problems: There can often be a significant delay in implementing this, due to professional opinion, allowing the patient to become severely malnourished. Healthcare professionals may fail to recognize that the problems are a direct consequence of very severe ME, preferring to postulate psychological theories rather than addressing the primary clinical need.
The study questionnaire recognised previously encountered difficulties experienced when researching severe ME. It considered the issues likely to prove a barrier to completing the document and tried to maximise participation, whilst reducing the risk of health deterioration.
The aims of the study were to explore whether, if the necessary support was provided and a modified extension to the usual timescale given, patients with very severe ME would be enabled to participate in research.
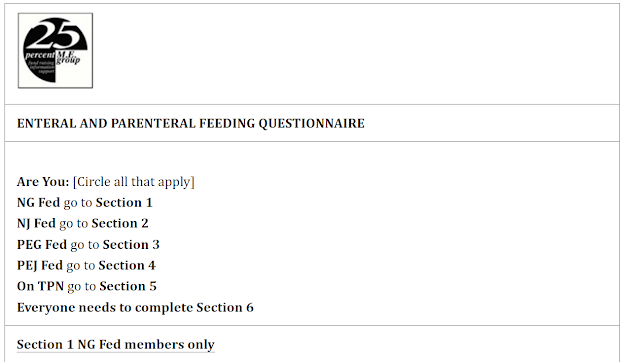
The Enteral and Parenteral Feeding Questionnaire by 25% ME Group in Appendix A below and within the 2022 paper outlining the difficulties for those with Severe and Very Severe ME in completing a survey on malnutrition, a survey entitled 'Ensuring the Voice of the Very Severely Affected Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patient Is Heard in Research—A Research Model, please see here
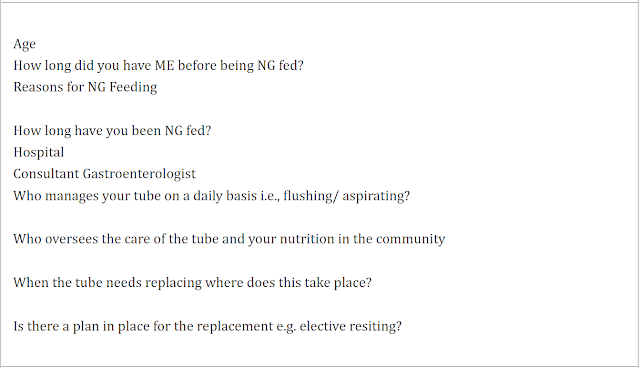 |
| Sections of the Enteral and Parenteral Feeding Questionnaire 2019 by 25% ME Group |
Trigger Warning: Please be aware of upsetting content ahead
Case 1 from the above linked study:
'This patient was diagnosed with severe ME as a child and has never fully recovered. She has been very severely affected for the past nine years. She has received care in a nursing home setting, hospital and now in her forties has around the clock care in the community.
Her difficulty swallowing started in 2015 whilst a resident in a nursing home. A speech and language therapist (SALT) diagnosed dysphagia, cause unspecified. A community dietitian visited and prescribed oral nutritional supplements (ONS). The patient was unable to tolerate these and became increasingly malnourished.
Although she was already significantly underweight, the primary health care team failed to recognize the severity of the situation. Over a seven week period she was almost completely unable to ingest any nutrition or hydration. As the situation deteriorated the patient was told that she would be sectioned under the Mental Health Act if she did not go to hospital. She reluctantly agreed to a voluntary admission.
Over a two week period in hospital she was intermittently given intravenous fluids, but no nutrition. She was screened using the malnutrition universal screening tool (MUST); her MUST score was 4 (2 or above denotes high risk of malnutrition [7]).
Her condition deteriorated further to the extent that she had to be admitted to a High Dependency Unit (HDU) because no Intensive Care Unit (ICU) bed was available, after which a Nasogastric Tube (NGT) was inserted. By this time, she was found to be suffering from a severe electrolyte imbalance, which further delayed the establishment of a feeding regime due to the risk of re-feeding syndrome.
Two months later with an established NGT feeding regime in place her MUST was still only 2.The patient gained the strong impression that her doctors regarded her problems as psychological in origin and that she was being treated as if she was suffering from an eating disorder.An NGT was sited prior to discharge. The patient was told another NGT would not be sited.
The tube remained in situ far longer than recommended until it became unusable. It was re-sited as an emergency in hospital. Subsequently the tube became blocked on several occasions and each time the patient had to attend the hospital as an emergency to have it replaced. This was especially concerning as there was no guarantee the tube would be re-sited, despite a clinical need.
In 2019 this situation improved after a Percutaneous Endoscopic Gastrostomy (PEG) was sited, and finally the patient had an improvement in her quality of life with the allocation of a Home Enteral Nutrition Service (HENS) dietician who made changes to the feed to ameliorate pain whilst being fed.
The patient still feels that there has been a failure to acknowledge her dysphagia. Today she has a normal BMI and continues to receive her preferred choice of care in the community.'
How to Support Patients with Malnutrition Problems
- From the 25% ME Group at The Malnutrition Task Force Sharing Practice Day:
"Our advocacy worker, Helen Baxter, did a talk on preventing avoidable malnutrition in severe ME at The Malnutrition Task Force Sharing Practice Day. The Malnutrition Task Force focus on malnutrition in the elderly and Helen has drawn on the comparisons between the nutrition and care needs of the elderly and people with severe ME."
Please see 12 minute video entiltled Preventing Avoidable Malnutrition in Severe ME
- Tube Feeding and Ability Scale from 'Severe ME/CFS A Guide to Living' by Emily Coleridge here


No comments:
Post a Comment